GLP-1 Patches: An In-Depth, Non-Promotional Overview
Introduction
Glucagon-like peptide-1 (GLP-1) has become a central topic in discussions around metabolic health, particularly in relation to type 2 diabetes, obesity, and appetite regulation. Traditionally, GLP-1–based therapies have been administered via injections or oral medications. More recently, interest has emerged around the idea of GLP-1 patches—transdermal systems designed to deliver GLP-1 or GLP-1–related compounds through the skin.
This article provides a comprehensive, non-promotional overview of GLP-1 patches. It explores what GLP-1 is, how it functions in the body, how transdermal delivery works, the scientific challenges involved, current research status, potential benefits, limitations, and unanswered questions. The goal is to inform rather than persuade, and to distinguish established evidence from emerging or theoretical concepts.
Understanding GLP-1: A Brief Biological Background
GLP-1 is a hormone classified as an incretin. It is naturally produced in the gut, primarily in the L-cells of the small intestine, and released in response to food intake. Its primary physiological roles include:
-
Stimulating insulin secretion in a glucose-dependent manner
-
Suppressing glucagon release
-
Slowing gastric emptying
-
Promoting satiety and reducing appetite
Because GLP-1 activity increases insulin release only when blood glucose levels are elevated, it plays a role in blood sugar regulation with a relatively low risk of hypoglycemia when functioning normally.
However, native GLP-1 has a very short half-life—only a few minutes—due to rapid degradation by the enzyme dipeptidyl peptidase-4 (DPP-4). This limitation led to the development of GLP-1 receptor agonists, which are modified compounds designed to resist breakdown and provide longer-lasting effects.
Conventional GLP-1 Delivery Methods
Before discussing patches, it is important to understand how GLP-1–based therapies are currently delivered.
Injectable GLP-1 Therapies
Most clinically approved GLP-1 receptor agonists are administered via subcutaneous injection. Depending on formulation, injections may be daily or weekly. This delivery route bypasses the digestive system, allowing large peptide molecules to enter the bloodstream intact.
Oral GLP-1 Formulations
Oral GLP-1 options exist but require specialized absorption enhancers to protect the peptide from stomach acid and enzymes. Even with these technologies, oral bioavailability remains relatively low, and dosing precision is complex.
Both methods are supported by extensive clinical trials. In contrast, GLP-1 patches remain an area of research and experimentation rather than widespread clinical practice.
What Are GLP-1 Patches?
GLP-1 patches are conceptualized as transdermal delivery systems designed to release GLP-1 or GLP-1–related compounds through the skin and into systemic circulation. Transdermal patches are already used for certain medications, such as nicotine, estrogen, and some pain medications.
The idea behind GLP-1 patches is to offer an alternative route of administration that could, in theory:
-
Avoid injections
-
Provide steady, controlled release
-
Improve convenience or adherence
However, the feasibility of delivering GLP-1 through the skin presents significant scientific challenges.
How Transdermal Drug Delivery Works
The skin is an effective barrier. Its outermost layer, the stratum corneum, is designed to prevent foreign substances from entering the body. While this is beneficial for protection, it complicates drug delivery.
Transdermal patches typically work best for substances that are:
-
Small in molecular size
-
Lipophilic (fat-soluble)
-
Potent at low doses
GLP-1 and GLP-1 receptor agonists are large peptide molecules, which are generally hydrophilic and poorly suited for passive skin absorption. As a result, conventional patch technology cannot easily deliver intact GLP-1 across the skin.
Technologies Explored for GLP-1 Patches
To overcome the skin barrier, researchers have explored several advanced techniques. These approaches are experimental and vary in effectiveness.
Microneedle Patches
Microneedle arrays consist of tiny, minimally invasive projections that create micro-channels in the skin. These channels allow larger molecules to pass through without causing significant pain or bleeding.
Microneedle patches are one of the most actively researched methods for transdermal delivery of peptides, including insulin and GLP-1 analogs. Some early studies suggest they can deliver biologically active compounds, but large-scale clinical validation is limited.
Chemical Penetration Enhancers
Certain chemicals can temporarily disrupt the stratum corneum, increasing skin permeability. While effective for some drugs, penetration enhancers may cause skin irritation and are less reliable for large peptides.
Encapsulation and Nanocarriers
Another approach involves encapsulating GLP-1 molecules in lipid-based carriers or nanoparticles designed to improve skin penetration. This area remains largely experimental, with ongoing investigation into safety, stability, and absorption consistency.
Current State of Scientific Evidence
As of now, GLP-1 patches are not widely approved medical treatments. Most evidence comes from:
-
Preclinical animal studies
-
Small human feasibility trials
-
Laboratory-based delivery research
These studies often focus on proof-of-concept rather than long-term outcomes. Compared to injectable GLP-1 therapies, there is a lack of large, randomized, controlled trials demonstrating consistent efficacy, safety, and dosing reliability for patch-based delivery.
This does not mean the concept is invalid, but it does mean that claims surrounding GLP-1 patches should be interpreted cautiously.
Potential Advantages (Theoretical)
If the technical challenges were successfully addressed, GLP-1 patches could offer several theoretical benefits:
-
Non-invasive administration
Avoiding needles may reduce anxiety and improve adherence for some individuals. -
Steady hormone release
Transdermal systems can provide more stable plasma concentrations, potentially reducing peaks and troughs. -
Convenience
Patches could simplify dosing schedules if designed for extended wear.
It is important to emphasize that these advantages are largely hypothetical at present and depend on future technological success.
Limitations and Challenges
The limitations of GLP-1 patches are significant and well-recognized in scientific literature.
Molecular Size and Stability
GLP-1 peptides are fragile and can degrade when exposed to heat, light, or oxygen. Maintaining stability in a patch format is technically demanding.
Absorption Variability
Skin thickness, hydration, temperature, and placement location all influence transdermal absorption. This variability makes precise dosing difficult, especially for hormones with narrow therapeutic windows.
Safety Considerations
Repeated skin penetration or chemical enhancement may lead to irritation, inflammation, or allergic reactions. Long-term skin safety data are limited.
Regulatory Hurdles
Because GLP-1 patches would involve novel delivery systems, regulatory approval would require extensive safety and efficacy data. This process is time-consuming and costly.
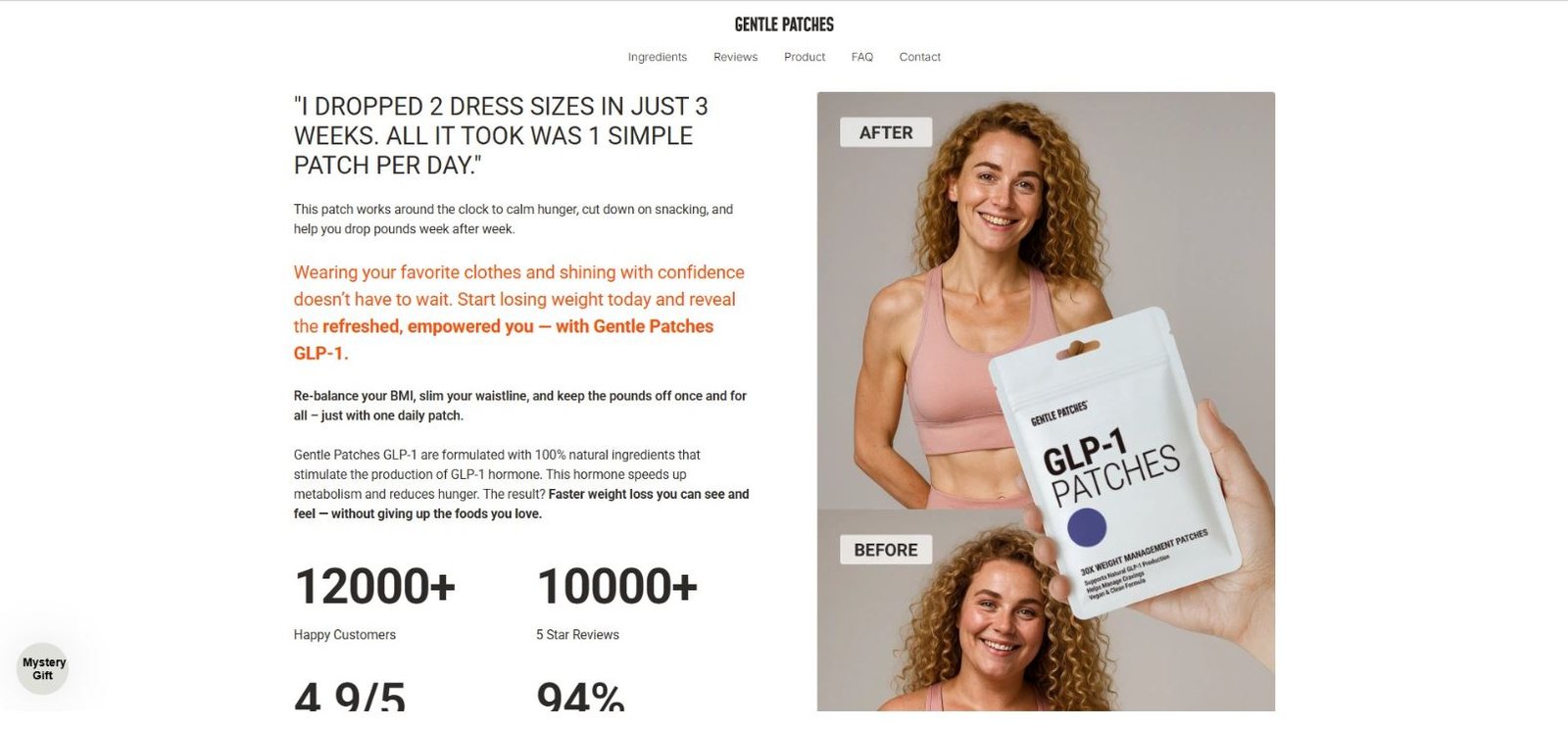
Distinguishing Prescription Therapies from Non-Prescription Products
An important point of confusion arises from the presence of non-prescription products marketed as “GLP-1 patches.” Many of these products do not contain GLP-1 or GLP-1 receptor agonists, which are prescription-only substances in many countries.
Instead, such patches may contain:
-
Plant extracts
-
Amino acids
-
Vitamins or minerals
While these ingredients may have general health roles, they do not replicate the pharmacological action of GLP-1 receptor agonists. From a scientific standpoint, these products should not be conflated with clinically studied GLP-1 therapies.
Ethical and Informational Considerations
The growing interest in GLP-1–related solutions highlights the importance of clear public understanding. Misinterpretation of early-stage research can lead to unrealistic expectations or misuse of unproven products.
From an ethical perspective, it is essential that:
-
Emerging technologies are accurately described
-
Limitations are clearly stated
-
Distinctions between research concepts and approved treatments are maintained
Health decisions should ideally be guided by peer-reviewed evidence and professional medical advice rather than novelty alone.
Future Research Directions
Research into GLP-1 patches continues, particularly in academic and pharmaceutical development settings. Areas of focus include:
-
Improved microneedle designs
-
Enhanced peptide stabilization methods
-
Better control of dosing accuracy
-
Long-term safety studies
It is possible that future innovations will make transdermal GLP-1 delivery more viable. However, timelines for widespread clinical use remain uncertain.
Conclusion
GLP-1 patches represent an intriguing concept at the intersection of hormone therapy and transdermal drug delivery. While the idea of delivering GLP-1 through the skin offers potential convenience and non-invasiveness, it also faces substantial biological, technical, and regulatory challenges.